CMS Rolls Out Prior Authorization Pilot Program for 2026
A new pilot program looks to introduce third-party management of prior authorizations in an effort to cut costs.

Subscribe
Get the latest news and tips directly in your inbox by subscribing to our monthly newsletter
Providers have long lamented prior authorizations, which have slowed down or halted care in the name of, let’s be honest, saving insurance companies money. For all of the problems with Medicare Part B as it exists now, which are too numerous to list here, one saving grace was that it didn’t impose those same hurdles, or at least to the degree that private payers have sought to gatekeep care by turning to utilization management companies. But that might soon be changing.
The Centers for Medicare and Medicaid Services (CMS) has announced a new pilot program, entitled the Wasteful and Inappropriate Service Reduction (WISeR) Model, that has a stated aim of rooting out waste and fraud within traditional Medicare. (Medicare Advantage would not be impacted, at least during the pilot program.) How are they achieving that goal? By hiring outside companies to use artificial intelligence and other “enhanced technologies” to streamline the prior authorization process for those services they’ve deemed as particularly apt for waste or fraud.
While there isn’t yet a full picture of how the program will operate, there are some details we can gather—not all of which may be comforting to providers. Prior authorizations won’t be solely driven by AI; the press release states that “while technology will support the review process, final decisions that a request for one of the selected services does not meet Medicare coverage requirements will be made by licensed clinicians, not machines.”
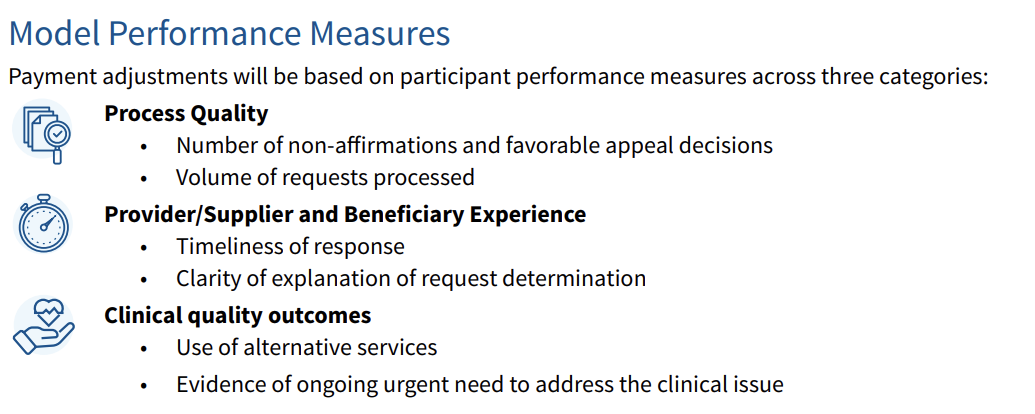
The release also details that while the program does not alter Medicare coverage and payment criteria, participants (the companies managing prior authorizations) will be paid based upon their ability to reduce “unnecessary” or non-covered services, as well as spending. These companies' payments will be adjusted based on their performance against quality and process measures that gauge their ability to support faster decisions for providers and “improve provider, supplier and beneficiary experience.” Below are the Model Performance Measures listed in the WISeR Model Factsheet:
Will rehab therapists be impacted? It’s as yet unclear which services this new model will be applied to, other than the fact that inpatient-only services, emergency services, and” services that would pose a substantial risk to patients if significantly delayed” are exempted. The initial rollout is limited as well; The Independent reports that the program is set to be introduced in six states beginning in 2026: New Jersey, Ohio, Oklahoma, Texas, Arizona, and Washington.
What might raise eyebrows is the fact that, as recently as this summer, Health and Human Services Secretary Robert F. Kennedy, Jr., and CMS Administratior Dr. Mehmet Oz secured a promise from private insurers to reduce and streamline prior authorizations. Place that against one of the stated goals from the WISeR Model’s website, which says that one aim is to “(a)pply commercial payer processes that may be faster, easier and more accurate” to Medicare. Given providers’ experiences with prior authorization, utilization management, and, frankly, private insurance as a whole, there will likely be plenty of skepticism as this program gets underway next year.





